Bloated and Breathless: The Connection Between Bloat and COPD
June 11, 2024
Content created for the Bezzy community and sponsored by our partners. Learn More
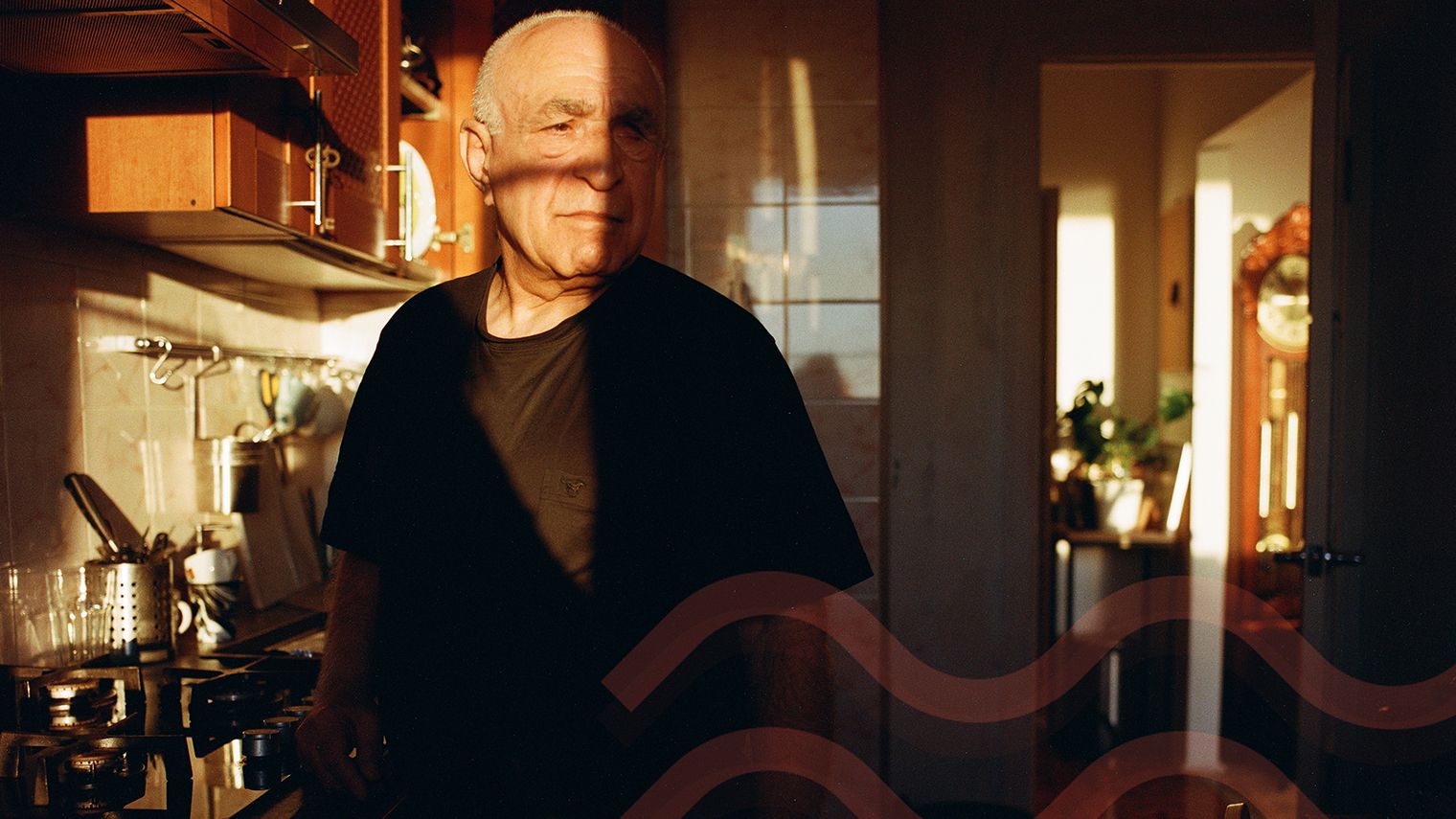
Photography by Lilith Matevosyan/Stocksy United
Bloating is a lesser-known symptom of COPD. Here are a few ways you can manage this uncomfortable issue.
Breathing, not digestive issues, is usually the main focus in COPD care. But gastrointestinal (GI) symptoms are common in people with COPD and have the potential to worsen as the disease progresses.
Why does that matter? Bloating can be painful and uncomfortable.
“Chronic pain from bloating can interfere with sleep, with eating enough, with travel in airplanes or to higher altitudes, and with the general enjoyment of life,” said David D. Clarke, MD, a clinical assistant professor of gastroenterology emeritus at Oregon Health & Science University in Portland, Oregon.
Clarke adds that you might feel severe cramping or like your stomach is stretching. It can even make it more challenging to breathe.
Understanding why COPD may increase your odds of experiencing GI discomfort, particularly bloat, and how to cope is important so that you can take care of yourself and enjoy activities you love.
I spoke with Clarke and other doctors who shared ways COPD can cause or worsen bloating and practical tips to reduce and prevent pain.


How does COPD cause bloat?
Consuming gassy foods like cruciferous vegetables, beans, and carbonated drinks can cause bloating in anyone. However, COPD can contribute to this uncomfortable symptom.
One study published in 2021 shows that GI symptoms are common in people with COPD and get worse as the disease progresses. Reasons include:
- airflow obstructions
- shallow breathing
- treatments for COPD and related conditions, like steroids or CPAP machines
- diet and how quickly you eat
- decreased physical activity
Airflow obstructions
“People with COPD often trap air in their stomachs and intestines,” said Nadeem Ali, MD, a pulmonologist at Meridian Health. “This trapped air causes the abdomen to shrink, leading to a feeling of fullness and discomfort.”
Shallow breathing
COPD also forces your body to take shallow breaths, which can also play a role.
“People with COPD sometimes tend to take shallow, frequent breaths, which may also lead to air swallowing, known as aerophagia,” said Bharat Pothuri, MD, a gastroenterologist at Memorial Hermann Hospital in Houston, Texas.
“People with COPD have elongated, expanded lungs, which can flatten the diaphragm. By doing this, it can push the upper digestive system forward, leading to abdominal distension,” he said.
Abdominal distension is the feeling of a swollen abdomen from air buildup, which can cause bloating.
Research, like a 2022 study including more than 500 people, shows an overlap between COPD and obstructive sleep apnea, a condition that can cause you to stop breathing while sleeping. A continuous positive airway pressure (CPAP) machine can reduce sleep apnea risks but might also increase bloating.
“Air from the machine can get sequestered in the stomach and cause bloating,” Pothuri said.
Treatments for COPD
To manage COPD itself, your doctor may prescribe steroids to reduce inflammation and clear your airways.
“A combination of this and increased food intake secondary to steroids can lead to bloating,” Pothuri said.
Diet and exercise
Foods like gassy veggies (think cabbage and broccoli) and bubbly drinks like soda and even seltzer can especially increase the odds of GI problems. Eating any food too quickly can as well.
While exercise is recommended for COPD, shortness of breath may leave you feeling like you need to move less because physical activity is challenging. Pothuri said that can increase your chances of GI issues, including bloating and constipation.
“All of these symptoms may be worsened if the patient has underlying digestive disorders, such as inflammatory bowel disease, irritable bowel syndrome, lactose intolerance, gastroparesis, or celiac disease,” Pothuri said.
Tips for busting bloat
The odds of experiencing bloating when managing COPD may be higher but aren’t guaranteed. Thankfully, there are ways to reduce your discomfort if you do become bloated.
By taking a few preventive and pain-relieving steps, you can focus on the activities that bring you joy and the people you love instead of belly bloat.
1. Practice breathing exercises
Breathing exercises are a main part of pulmonary rehabilitation because they can improve COPD symptoms, including bloating.
“Focus on breathing through the nose rather than mouth breathing, as this can help reduce the amount of air that is pulled down the esophagus, which is the muscular tube between the throat and stomach,” Clarke said. “Practicing slow, controlled breathing may also provide relief.”
2. Diet
Of course, what goes into your stomach can affect how it feels. There are certain foods Pothuri advises against.
“Avoid artificial sweeteners, chewing gum, carbonated beverages, beans, broccoli, cauliflower, and cabbage,” Pothuri said.
We always hear broccoli and beans are nutritious. They are, and they add much-needed fiber to your diet. But they can also create unwanted gas in your abdomen.
Pothuri doesn’t suggest cutting out these gut-healthy greens and beans completely. Instead, he suggests eating them slowly and taking the time to chew your food. Small, frequent meals also offer slower digestion. Another tip is to drink plain water, not carbonated.
As for hydration, the Centers for Disease Control and Prevention (CDC) recommends considering your health status, activity level, and climate when deciding how much water to drink. But as with any recommendation, it’s best to ask your doctor for advice.
3. Evaluate your medications
If lifestyle tweaks don’t work, treatment options are available, including bloating-specific remedies and switching medications for COPD management.
“Try over-the-counter medications like simethicone that can break up gas bubbles and make it easier to pass gas,” Clarke said.
Several studies have shown that simethicone can reduce bloating, such as a 2019 meta-analysis and review of research involving more than 5,000 people. However, the research didn’t involve people living with COPD.
Pothuri said speaking with your care team about alternatives to steroids and narcotics with fewer GI-related side effects can also reduce how bloating affects your life.
4. Increase your physical activity
While it’s understandable that you may be hesitant to exercise because of shortness of breath, doctors often recommend it as part of a treatment plan. Like breathing exercises, it’s also part of pulmonary rehabilitation. It also helps improve bloating.
“Increase physical activity with light exercise like walking 30 to 90 minutes after a meal, as this can help pass trapped gas and relieve bloating,” Clarke said.
Exercise doesn’t have to be intense. Your care team may recommend gentle chair exercises.
5. Address other conditions
Since bloating related to COPD can be worsened by other health conditions, Clarke recommends speaking up at your next appointment. It could be a sign of something else.
“If bloating persists despite these measures, further evaluation may be needed to rule out other contributing factors like irritable bowel syndrome, constipation, sleep apnea, or any of several sources of stress, including current life stresses, mental health conditions, and the long-term impact of adverse childhood experiences,” Clarke said.
When to call a doctor for COPD and bloating
COPD can cause or worsen bloating, but sometimes, it’s best to rule out other options. You should always feel comfortable expressing concerns to your doctor, but Ali said it’s especially important if you’re also experiencing:
- chest pain
- shortness of breath
- wheezing
- coughing up blood
- swelling in your ankles or feet
- fatigue
- weight loss
Takeaway
COPD and bloating can overlap. Swallowing air from shallow breathing, eating too fast, and treatments for COPD and other conditions, like sleep apnea, can all prompt bloating.
Bloating is something people can experience whether they have COPD or not. Still, it can be uncomfortable and even worsen breathing problems, which can be incredibly distressing.
You should always feel comfortable speaking with doctors about your concerns. No issue is “too minor,” and you don’t need to “tough it out.”
Lifestyle tweaks, like breathing modifications and exercise, drinking water after meals, and over-the-counter medications to reduce bloating, can all help.
Medically reviewed on June 11, 2024
7 Sources


Like the story? React, bookmark, or share below:
Have thoughts or suggestions about this article? Email us at article-feedback@bezzy.com.
About the author